
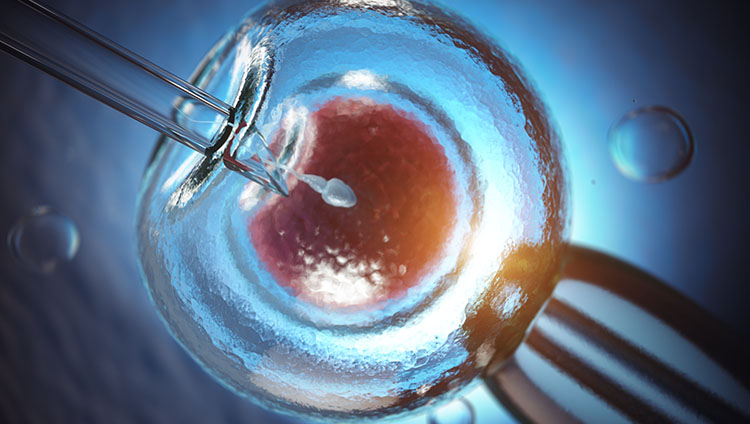
TESE, the procedure for obtaining sperm from the testicles to be injected into the egg via a micromanipulator, has been a great opportunity for azoospermic men who do not have a normal sperm output. About half of such cases became fathers thanks to testicular sperm. Apart from severe cases, pregnancy success does not differ significantly from naturally produced sperm. Moreover, when it has been shown in recent years that it is possible to have children with immature early-stage sperm cells, the importance of testicular sperm has increased even more.
The most reliable and healthy way to collect sperm from the testis is the microTESE technique, that is, the investigation of the sperm-containing tubules using microsurgical instrumentation under the operating microscope. In the surgery performed with this technique, tissue loss will be minimal and there will be no significant change in blood testosterone level. TESE can be done without using a microscope, but in this case, more tissue samples must be taken. The more tissue is removed, the more damage is done to the testis. Another issue that is curious about this issue is how many times TESE surgery can be performed at most. If the microTESE method has been used, there is no harm in repeating it several times. Moreover, if sperm were searched for with a simple biopsy technique before, when microTESE is performed again later, mature, live sperm can be obtained in nearly half of the cases.
More than 20 years have passed since microTESE surgery was first performed. However, in the last few years, there have been new developments that have made the TESE procedure more efficient. In the light of new developments, we have now expanded the classical TESE process by further detailing, and therefore we have chosen to define it as "multi-directional microTESE". Accordingly, we recommend that certain steps be followed when TESE is planned in an azoospermic patient with impaired sperm production in the testicles:
1. Demonstrating with markers that there is no absolute deficiency in the genetic material responsible for sperm production in testicular stem cells.
2. Supporting these cells for at least one sperm cycle with specific appropriate medication.
3. In the final stage, making sure that spermatogenic cells suitable for ICSI/ROSI have developed in the testis by using seminal markers.
4. Performing the microTESE attempt and searching for mature sperm cells with tail development or immature early stage sperm cells with insufficient tail development, freezing the collected cells.
5. Demonstrating by genetic studies that the cells taken are healthy haploid sperms that have completed meiosis.
6. Preparing the partner and going to in vitro fertilization with ICSI or ROSI technique according to the tail development level of the cells.
7. If necessary, genetic screening of the resulting embryos with PGD.
8. Careful pregnancy follow-up.
When in vitro fertilization is performed after passing these stages, fertilization occurs at a rate of 90-95%, and pregnancy can be achieved in 5% to 40% depending on the maturity level of the processed cells. Despite everything, it should be noted that 2-3% of all IVF attempts may develop a pregnancy with minor or major congenital anomalies. However, each case is unique and therefore both spouses should be examined very carefully and a good information should be given. The aim is not to do IVF, but to give birth to a healthy child.
You can send your questions to
Prof.Dr. Kaan Aydos
Mahatma Gandhi Caddesi, 19/7 06700 Cankaya, Ankara / TURKEY
+90 312 437 3121 +90 312 508 2258